Genetic testing could lower the risk of adverse drug reactions for thousands of patients with cancer
A new study led by Genomics England and Queen Mary University of London estimates that genetic testing could identify approximately 14,540 patients per year on any of 5 commonly prescribed drugs who could potentially benefit from a reduced dose or alternative drug to reduce the risk of adverse drug reactions – or harmful side effects - which can be fatal.
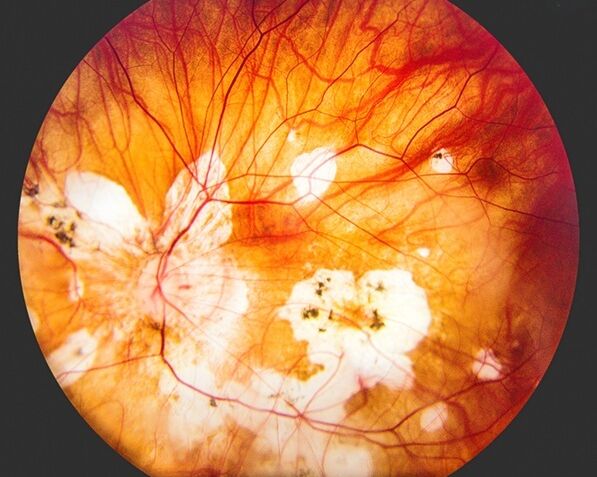
The research, published today in the Journal of Clinical Oncology, analysed whole genome sequencing results from 76,805 participants from the 100,000 Genomes Project. The researchers looked at pharmacogenetic variants – genetic changes that affect our bodies’ handling of and response to drugs - in 4 genes that are known to be linked to harmful reactions to 5 drugs commonly used in cancer treatment. Patients’ genomic data was linked with prescribing data as well as hospital incidence records to identify whether patients with certain genetic alterations suffered an adverse drug reaction after being prescribed their cancer drug.
The results showed that 62.7% of patients had a genetic variant that increased their risk of an adverse drug reaction when treated with one of the five common cancer drugs examined. For each drug investigated, between 6-10% of patients could benefit from either a reduced dose or a different drug altogether. Genetic testing for one of the 4 genes studied – a gene called DPYD – is already available through the NHS Genomic Medicine Service.
By extending the findings to annual prescription numbers in England for the drugs affected by the variants studied, approximately 14,540 patients per year could potentially lower their risk of adverse drug reactions through a reduced dose or alternative drug.
Adverse drug reactions account for one in 16 hospital admissions. They have been estimated to cost the NHS between £500 million and £2.2 billion annually.
Almost 99% of people carry at least one genetic variation that affects their response to certain drugs, underscoring the importance of pharmacogenomics (study of the genome’s role in drug response).
The study also shows the benefit of pharmacogenomics from whole genome sequencing to clinical decision making, as well as the potential positive impact it can have within the NHS.
“This has been a collaborative effort to effectively detect, analyse, interpret and feedback these key variants from whole genome sequences to patients.
“Cancer treatment by its nature of killing cells is often associated with unwanted side effects, however if we can reduce the risk of severe adverse reactions through identifying patients most at risk, patients are more likely to stay on treatments and be treated more effectively.
“We hope by showing the potential impact of pharmacogenetic results for cancer patients as well as at a population level, this will pave the way for making pharmacogenomics a part of future clinical practice, helping prevent dangerous side effects and lead to more personalised healthcare for patients.”
Dr Ellen McDonagh
Lead author of the paper
“Using whole genome sequencing to ensure patients with cancer get the right drug, at the right dose, at the right time, can make a considerable difference to ensuring they receive not only quick but also safer and more effective treatment.
“The UK is already a world leader in genomic medicine, and mastering pre-emptive pharmacogenomics will enable us to do even more for patients."
Professor Matt Brown
Chief Scientific Officer at Genomics England
“This study demonstrates the power of whole genome sequencing to improve treatment outcomes for patients with cancer. By integrating whole genome sequencing into cancer treatment, we have the power to transform cancer care from a ‘one size fits all’ approach to a personalised approach for each individual patient.”
Professor Sir Mark Caulfield
VP Health at Queen Mary University of London
"Facing cancer treatment is never easy. Many patients are willing to endure side effects for the chance to live a longer and meaningful life. But no one wants their treatment to make them seriously ill.
“Understanding when to lower the dose or avoid certain treatments altogether is crucial in minimising the risk of severe side effects or even fatal outcomes for those undergoing cancer treatment.
“By personalising treatment based on their genetic makeup, cancer patients can be offered safer and more effective options, providing much-needed hope for better outcomes and a chance to live longer, healthier lives."
Helen White
Vice Chair for Cancer, Genomics England Participant Panel