Genetic study gives extensive insights into severe COVID-19
The world’s largest study of the genetics of critical COVID-19, involving more than 57,000 people, has revealed fresh details about some of the biological mechanisms behind the severe form of the disease.
Some 16 new genetic variants associated with severe COVID-19, including some related to blood clotting, immune response and intensity of inflammation, have been identified.
These findings will act as a roadmap for future efforts, opening new fields of research focused on potential new therapies and diagnostics with pinpoint accuracy, experts say.
Researchers from the GenOMICC consortium – a global collaboration to study genetics in critical illness – led by University of Edinburgh in partnership with Genomics England, made these discoveries by sequencing the genomes of 7,491 patients from 224 intensive care units in the UK.
Their DNA was compared with 48,400 other people, including 46,770 who had not had COVID-19, participants in Genomics England's 100,000 Genomes Project, and 1,630 people who had experienced mild COVID-19.
Determining the whole genome sequence for all participants in the study allowed the team to create a precise map and identify genetic variation linked to severity of COVID-19. The team found key differences in 16 genes in the ICU patients when compared with the DNA of the other groups.
They also confirmed the involvement of seven other genetic variations already associated with severe COVID-19 discovered in earlier studies from the same team.
The findings included how a single gene variant that disrupts a key messenger molecule in immune system signaling – called interferon alpha-10 – was enough to increase a patient’s risk of severe disease.
This highlights the gene’s key role in the immune system and suggests that treating patients with interferon – proteins released by immune cells to defend against viruses – may help manage disease in the early stages.
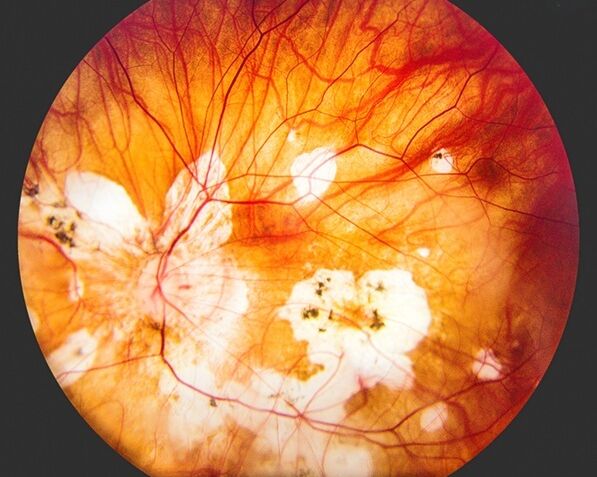
The study also found that variations in genes that control the levels of a central component of blood clotting – known as Factor 8 – were associated with critical illness in COVID-19.
This may explain some of the clotting abnormalities that are seen in severe cases of COVID-19. Factor 8 is the gene underlying the most common type of haemophilia.
Our latest findings point to specific molecular targets in critical Covid-19. These results explain why some people develop life-threatening Covid-19, while others get no symptoms at all. But more importantly, this gives us a deep understanding of the process of disease and is a big step forward in finding more effective treatments.
“It is now true to say that we understand the mechanisms of Covid better than the other syndromes we treat in intensive care in normal times – sepsis, flu, and other forms of critical illness. Covid-19 is showing us the way to tackle those problems in the future.”
Professor Kenneth Baillie (Chief Investigator)
Consultant in Critical Care Medicine at University of Edinburgh
As Covid-19 evolves, we need to focus on reducing the number of people getting seriously ill and being hospitalised. Through our whole genome sequencing research, we’ve discovered novel gene variants that predispose people to severe illness – which now offer a route to new tests and treatments, to help protect the public and the NHS from this virus.”
Professor Mark Caulfield (co-author)
Queen Mary University of London, formerly Chief Scientist at Genomics England
Strategically, we’re at a point where genomic science is becoming an integral part of the national infrastructure in routine healthcare. This study illustrates the value of whole genome sequencing to detect rare and common variants that influence critical illness requiring intensive care. It represents a major leap forward in our understanding of how our genetic makeup influences severe illness with Covid-19.”
“All those involved in the study went to great efforts to engage with all communities within the UK – including groups that have historically been under-represented in medical studies. The inclusive element of our work has generated meaningful results for everyone in the country.”
Dr Rich Scott
Chief Medical Officer at Genomics England
Clinical research has been vital in our fight against Covid-19 and the UK’s innovation is enabling us to transform our health service and ensure the NHS is able to deliver world-class care.
“This research is an important step forward in better understanding how Covid-19 impacts certain people, allowing us to take the necessary action to protect the most vulnerable and save lives.”
Lord Kamall
Minister for innovation at the Department of Health and Social Care (DHSC)
We’re delighted to have supported this exciting study that reveals more about the genetic profile of people who get critically ill with Covid-19.
These studies are important because they not only reveal important genetic factors that drive severe disease, but they could also highlight potential future treatment options for Covid-19, either through new drugs or existing drugs that could be repurposed. We are proud to be supporting the programme by helping the team decide which drugs to investigate and take forward.
We’ll watch with interest as these discoveries advance the therapeutics pipeline towards the clinic, where they could ultimately help patients.
Dr Dave Powell
LifeArc’s Chief Scientific Officer
The GenOMICC study has been a key part of the UK's urgent public health research response to the Covid-19 pandemic. The scale and speed of recruitment to this important study has been enabled by the National Institute for Health Research's Clinical Research Network - which mobilised its workforce across every NHS trust in the country. Once again, the research community in the UK has delivered results that have the potential to change clinical practice and save lives across the world.
Professor Nick Lemoine
National Institute for Health Research
These findings show the power of whole genome sequencing which has uncovered new treatment targets for severe Covid-19.
Professor Patrick Chinnery
Clinical Director at the Medical Research Council
Illumina is very pleased to be part of this public-private consortium, which came together early in the pandemic to tackle a key healthcare question; we are delighted to witness the power of human whole genome sequencing in revealing important new insights into why some patients have severe responses to Covid-19. This is a unique study which demonstrates how the application of genomics medicine delivers the ability to predict patient response to coronavirus infection, and paves the way for the development of novel targeted treatments.
Dr David Bentley
Vice President and Chief Scientist, Illumina
ICNARC is proud to have collaborated in this important research that not only demonstrates the value of whole genome sequencing to reveal the mechanisms and potential treatment options for people with COVID-19 but also illustrates the power of linked data to explore and understand genetic influences that lead to some people becoming critically ill – a major step as we now need to move forwards in tackling sepsis, influenza and other major critical illnesses.
Professor Kathy Rowan
Director of Intensive Care National Audit and Research Centre (ICNARC)
This study using whole genome sequencing has paved the way for major advances in our understanding of why some people have very severe illness with COVID-19. The study strongly compliments COG-UK’s viral sequencing programme by providing the human genomic architecture of critical illness. In the future, combining the clinical and human and viral genomic environment will offer the chance to highlight novel interventions that minimise the impact on humanity from COVID-19.
Professor Sharon Peacock
Director of the COVID-19 Genomics UK (COG-UK) Consortium
The findings have been published in Nature.
GenOMICC (Genetics of Susceptibility and Mortality in Critical Care) started in 2015 as an open, global consortium of intensive care clinicians dedicated to understanding genetic factors influencing outcomes in intensive care from diseases such as SARS, flu and sepsis.
The consortium is led by the University of Edinburgh, and since 2020 it has been focused on Covid-19 research in partnership with Genomics England and in collaboration with NHS Lothian, the Intensive Care National Audit and Research Centre (ICNARC), and Queen Mary University of London.
The ground-breaking 100,000 Genomes Project was established in 2014 to sequence 100,000 genomes from people with a rare disease or cancer. The Project was completed in 2018 and paved the way for the creation of a new genomic medicine service for NHS England, transforming patient care by bringing advanced diagnosis and personalised treatments.
GenOMICC is funded by DHSC, LifeArc, the charity Sepsis Research FEAT, the Intensive Care Society, Wellcome, UK Research and Innovation, Scotland’s Chief Scientist Office, the Department of Health and Social Care and the National Institute for Health Research (NIHR), and supported by Illumina.