The journey to 100,000 genomes
Genomic potential
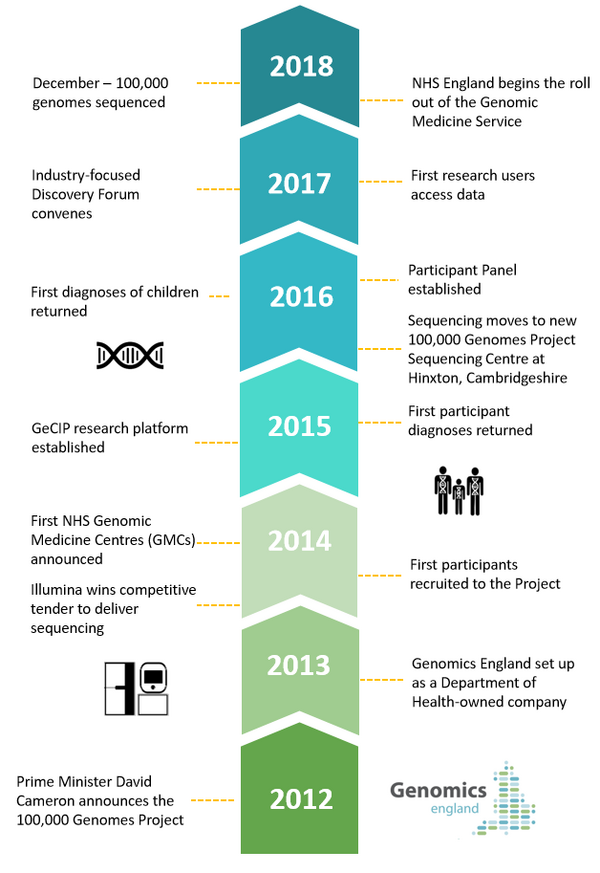
Pinpointing the beginning of the 100,000 Genomes Project isn’t easy. It could be argued that Crick, Franklin and Watson started it all in 1953; or Frederick Sanger’s pioneering sequencing technologies in the late ‘70s; perhaps the Human Genome Project in 2003; or even the UK10K project in 2008. Our journey, however, began in 2012 with the announcement of the Project and, in 2013, the creation of Genomics England to drive it to completion.
The background to the odyssey was a recognition that advances in genomics, informatics and analytics brought closer the possibility of more precise diagnosis, alongside personlised and targeted treatments. In 2012 science could see the potential to identify the underlying cause of disease, predict how a person might respond to specific interventions and determine who was at risk of developing an illness.
The stumbling block? Nobody had ever tried.
The UK was brave enough to lead the way – announcing the groundbreaking 100,000 Genomes Project, which aimed to sequence 100,000 whole genomes from around 70,000 participants with rare disease, their families and people with some cancers. The decision was backed by robust government support – both political and financial – which included over £300 million of investment.
Building a genomic infrastructure – partnership on an industrial scale
As we celebrate the sequencing of the 100,000th whole genome just five years later, it is important to remember the scale of the achievement. For those of us here at the beginning, the prospect was simultaneously exciting and daunting. We were asked to not only sequence an unprecedented number of whole human genomes, but also to plug this in to the rich health data held by the NHS. With important objectives to create a consent-based and transparent programme that fostered an emerging UK genomics industry – our ultimate aim was to bring real and lasting change to NHS care.
The challenge, described by one colleague as “building the plane whilst flying it”, was to create the infrastructure for genomic medicine from scratch, whilst also delivering on our objectives. A more traditional model would have seen us build the machinery first and then begin sequencing: the 100,000 Genomes Project did both simultaneously. It was a Project that demanded partnership on an industrial scale – and would never have been delivered without the support of thousands of organisations and individuals.
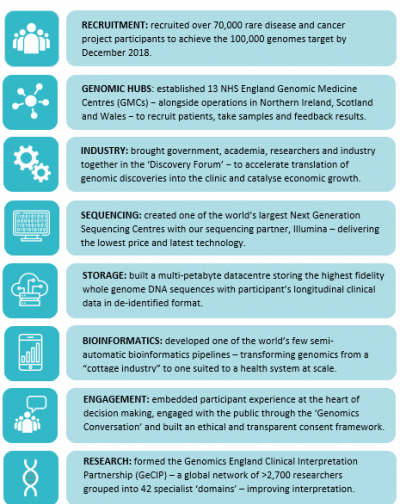
Genomics England began its close relationship with NHS England to recruit the first participants in 2014. In the same year, NHS England created 11 Genomic Medicine Centres (GMCs), eventually growing to 13 in 2015, and today joined by organisations in Northern Ireland, Scotland and Wales.
GMCs work across areas of 3 to 5 million people in over 85 NHS trusts. They have been key components of the project: recruiting and consenting patients; providing DNA samples; developing the mechanisms for validating results; and working to feed back results to participants. We cannot underestimate the commitment, skill and hard work of thousands of NHS staff who have pioneered these GMCs and the cause of genomic medicine in the NHS.
At the start of 2015, another piece of the infrastructure puzzle fell into place with the opening of the NIHR Biosample Centre to store samples from the Project. And just two months later, we established the Genomics England Clinical Interpretation Partnership (GeCIP). GeCiP brings together thousands of researchers and clinicians from across the world – granting them carefully controlled access to our database to power new discoveries in genomic medicine. Today GeCIP research covers 42 areas – known as ‘domains’ – including rare cardiovascular and neurological disorders, and cancers such as breast, lung and ovarian.
Early in the Project, we realised that many of the technologies and services needed to deliver genomic medicine simply didn’t exist – and if we wanted them we would have to build them. One of these technologies was the bioinformatics pipeline, which is critical to ensure processing at the scale in the world’s largest publicly funded health system. It has involved a huge commitment from our bioinformatics team and others – but has resulted in one of the world’s few semi-automatic bioinformatics pipelines.
This ‘if you can’t buy it, build it’ approach has seen a range of innovations. Work with our sequencing partner, Illumina, for example has acted as a significant catalyst in reducing the costs of sequencing: from billions in 2003 to around £600 today and around £100 in the not too distant future. We have also created a bespoke, multi-petabyte storage environment to cope with the grand challenge of managing a large scale whole genome and clinical dataset.
In 2015 we also began to explore how to align our work with the needs of industry – the companies that will eventually turn genomic discovery into routine treatments. This started with the GENE Consortium, which evolved in 2017 into the Genomics England Discovery Forum we see today. The Forum is a platform that allows us to bring together charities, patients, researchers, clinicians and others with industry partners to share perspectives and better understand how to speed discoveries from the laboratory bench to the patient’s bedside. In the past few months, the value of the Forum has been demonstrated with members discovering previously undiagnosed patients in our database – with the hope that this will lead to better diagnosis and the development of more effective treatments.
People powered healthcare
From the outset, the Project recognised that genomic medicine could not succeed without the understanding, trust, acceptance and consent of patients. Genomic medicine is truly “people-powered healthcare”. It heralds a changing relationship between the patient and the NHS, with a new consent model where healthcare and research become indivisible. It is important to understand that new technology and the use of data will only be socially and clinically enabled if it is trusted by the patient.
In 2016 Genomics England established the Participant Panel, which acts as an advisory body to our Board. The Panel is at the heart of our decision making processes, with members sitting on the Access Review Committee, the Ethics Advisory Committee and the GeCIP Board. Involving participants at this fundamental level ensures that the Project is always responsible to the people who drive it.
It also underlines the importance of the Project to participants. Participant Panel Deputy Chair, Rebecca Middleton, has said, “The Project brings me something new – hope. Whether in 5 or 15 years, new genomic discoveries may be able to help me.”
Ensuring that we are able to gain the trust of patients demands that we understand their attitudes to genomic medicine – and this inspired the ‘Genomics Conversation’ in 2016. The Conversation is a genuine engagement project – not seeking to influence its audiences, but rather to listen.
And what is it that patients get from the investment of their trust, understanding and consent?
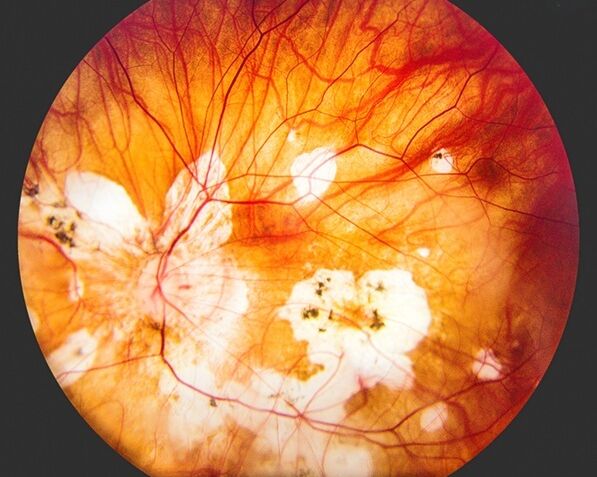
Even at this early stage, genomic medicine is helping to transform cancer services – making real progress in providing DNA of sufficient quality for whole genome sequencing – an issue that has hampered efforts to apply genomics in cancer diagnosis and treatment around the world. NHS England is re-aligning its laboratory services as it moves from formalin-fixed paraffin embedded (FFPE) to Fresh Frozen (FF) sample handling.
The first participants received their diagnoses in February 2015, when we had sequenced around 2,000 whole genomes, with the first diagnosis of children made in January 2016.
As we have moved to 100,000 genomes, the number of people has grown. People like Project participant Alexander and his family who in finally receiving a diagnosis for LEOPARD Syndrome can now finally know what is wrong and seek support from others living with the same disease. Fellow participant, Jessica, and her family discovered that her condition is caused by errors in the SLC2A1 gene that cause ‘Glut1 deficiency syndrome’ – which only affects around 500 people worldwide. Jessica’s diagnosis has opened up the potential for highly tailored treatments.
Beyond 100,000 genomes
The 100,000 Genomes Project has been a real innovation – from bioinformatics to computing to storage to research to industry partnership to public engagement. As our learning and dataset grows, so too will our ability to better diagnose and treat an ever expanding number of diseases. Whilst the UK is now an acknowledged leader in population genomics, this is a truly global effort – with the potential to bring patient and economic benefit across the world.
The Secretary of State of Health and Social Care’s announcement on 2 October laid out an exciting roadmap for genomic medicine. His words demonstrate the importance of personalised medicine and its ability to continue to deliver cutting edge care within the NHS: “I’m proud to announce we are expanding our 100,000 Genomes Project so that one million whole genomes will now be sequenced by the NHS and the UK Biobank. I’m incredibly excited about the potential for this type of technology to improve the diagnosis and treatment for patients to help people live longer, healthier lives – a vital part of our long-term plan for the NHS.”
The lasting legacy of the 100,000 Genomes Project is the NHS Genomics Medicine Service that began to roll out at the beginning of October 2018. The Project has proven the concept of genomic medicine at scale and built the infrastructure that underpins the GMS. Genomics and the GMS are transformative, poised to change the way future of healthcare is delivered. As we reach the 100,000 genome milestone, we are at a tipping point in medicine that will usher in an era of highly personalised medicine – which may consign generic drugs and treatments to medical history.
Getting to this point has been a demonstration of the power of partnership. We are only here because of the thousands of patients and their families who have placed their trust in a project at the cutting edge of healthcare. Working with them have been many thousands of NHS staff who worked tirelessly to not only deliver the Project, but in many cases, pioneer totally new systems, processes and procedures to ensure that genomic medicine can become part of routine NHS care. And beyond them there is the vast and rich ecosystem of charities, industry partners, funders, government organisations and a host of others. To everyone – we would like to say “thank you”.
Whatever its history and whenever it began, we can be sure that the genomic medicine journey is just beginning – and its future will be an exciting one.