Baby with rare eye cancer diagnosed and receiving lifechanging treatment earlier after genomic sequencing at birth

A boy born with a rare form of eye cancer, usually diagnosed in very young children, is one of numerous babies born with rare conditions who are receiving earlier diagnoses and faster, lifechanging treatment through the Generation Study - a world-leading research study led by Genomics England in partnership with NHS England that is using whole genome sequencing to screen 100,000 newborns and look for more than 200 rare genetic conditions.
Completing the Generation Study is a key part of England’s 10 Year Health Plan. The findings will help inform the Government’s long-term ambition to offer genomic sequencing to all newborns as part of routine care - making it possible to detect and treat serious conditions early in life. This ambition will be subject to the important evidence and data the Generation Study gathers.
So far, over 20,000 participants have joined the study and more than 60 ‘condition suspected results’ have been returned by Genomics England to the NHS for confirmatory testing.
‘Our decision to join the Generation Study has changed Freddie’s life phenomenally’
Vicky and Joey Underhay’s son, Freddie, is one child who has benefitted from being part of the study.
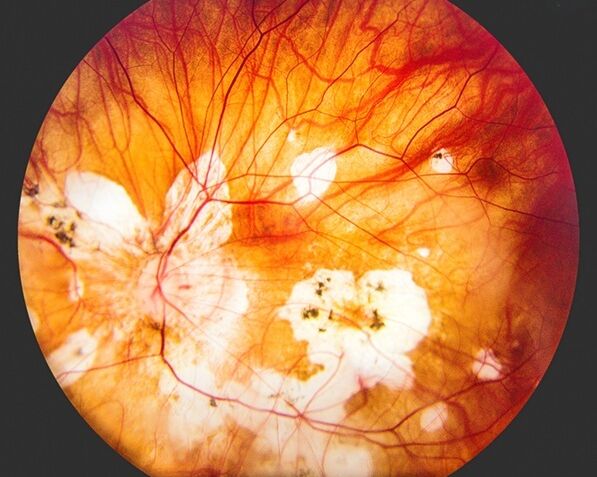
Four weeks after being born at the Jessop Wing at Sheffield Teaching Hospitals NHS Foundation Trust in April and having his genome sequenced, Freddie was diagnosed with hereditary retinoblastoma, caused by a change in his RB1 gene. Retinoblastoma is a rare and aggressive form of eye cancer usually diagnosed in very young children. Around 44 children are diagnosed with retinoblastoma every year in the UK, and early detection is crucial for preserving vision. However, when there is no known family history, diagnosis often comes later, once symptoms have progressed.
Vicky Underhay said: “There were no signs that anything was wrong. He was a normal little baby, so the results came totally out of the blue. He had passed all his eye tests in hospital.”
Very shortly after his diagnosis, Freddie was able to start treatment at Birmingham Children's Hospital, which is one of two specialist centres that treat retinoblastoma in the UK. This gives doctors the best chance to minimise the impact on his vision.
Freddie has undergone a mix of chemotherapy and laser treatment to treat the tumours in his eyes. Due to the nature of retinoblastoma and the genetic change involved, Freddie will need ongoing treatment, monitoring, and specialist care for the foreseeable future. He will be having regular eye screenings up until the age of 16 in Birmingham.
Joey Underhay said: “Our decision to join the Generation Study has changed Freddie’s life phenomenally. We were told that the first 6 months is vital in diagnosing and treating the condition. There’s no telling at what point it would have been discovered if we hadn’t taken part and what might have happened.
“The care that Freddie has received, and us as parents as well, has been second to none. We can’t thank everyone enough for all that they’re doing for Freddie.”
Vicky Underhay added: “When you sign up to research like this, you think it will never be you. But if we had thought ‘ignorance is bliss’ then the cancer would have spread down his optic nerve and into his body. We’re hopeful that this kind of testing will be readily available to any parent who wants it for their child in the future.”
Dr Joe Abbott, Freddie's ophthalmologist, said: “The chances of protecting Freddie's eyesight have been greatly improved by finding out about his eye tumours earlier, thanks to the family participating in the Generation Study.”
Study progress
The Generation Study is currently available in 51 different hospitals in England.
It is offering participating families whole genome sequencing for their baby using blood samples taken shortly after birth. Whole genome sequencing is a technique used to read all of someone’s DNA to understand their genetic makeup. The Generation Study is looking for more than 200 rare conditions which usually appear in the first few years of life, can be improved if caught early, and can be treated in the NHS.
While the whole genome is sequenced, the study is only looking for changes in genes that are expected to cause a defined list of 200+ rare conditions.
The study, which launched in 2024 and will run until 2027, has already identified numerous conditions - allowing those babies to receive vital treatment at an earlier stage that can slow their condition’s progression or stop them from becoming ill. Around 1% of babies in the study will be suspected to have a condition, which is then confirmed with follow-up testing in the NHS.
More preventative healthcare
“We believe genomics can transform healthcare in this country and be used to get ahead of serious illness. It’s been incredibly moving to see the lifechanging impact the Generation Study is having for families like Freddie’s, who have been able to access treatment that makes a world of difference soon after being born.
“Every year thousands of babies are born in the UK with rare genetic conditions, but they can be hard to diagnose. On average, it takes around five years for a rare condition to be diagnosed, at which point it has often progressed to the point where treatment, if it exists, is far less effective.
“We’re fortunate that UK is uniquely placed to test and – if the evidence supports it – roll out genomic innovations that help us move towards preventing sickness, not just treating it. The Generation Study is an example of just that – a national-scale research study developing evidence to inform whether every baby should be offered genomic sequencing. It’s an important step towards a future of healthcare that is more preventative, with genomics playing a key role in that throughout someone’s life.”
Dr Rich Scott
Chief Executive Officer of Genomics England
“This is exactly the kind of preventative healthcare that this government is committed to delivering for families across England. Stories like Freddie's show the incredible potential of genomic medicine to catch serious conditions early, when treatment can be most effective.
“Our 10 Year Health Plan places genomics at the heart of a transformed NHS and by potentially offering genomic sequencing to all newborns in future, we're moving towards a healthcare system that prevents illness rather than just treating it.
“This study represents the best of British innovation in healthcare - using cutting-edge science to give children the best possible start in life. It's a vital step in our vision of an NHS that is fit for the future.”
Zubir Ahmed
Health Innovation Minister
“Today’s announcement is a major step forward for the NHS in the use of whole genome sequencing in newborns.
“Freddie’s amazing story highlights the strength of our world leading partnership with Genomics England, showing it is possible to identify rare genetic conditions like these earlier so children can start treatment faster meaning they have the best chance of a cure.”
Professor Dame Sue Hill
Chief Scientific Officer for England
“Early diagnosis and access to treatment can be truly life-changing for families affected by rare conditions – it’s why we’re so excited by the Generation Study and its potential to help families across the country.
“The Participant Panel shares Genomics England’s commitment to help everyone benefit from genomic healthcare, and we hope the evidence generated through the Generation Study will help progress this. We look forward to continuing working with Genomics England and ensuring participants' interests remain at the core of all activities, aided by greater public and patient involvement and engagement in research.”
Kirsty Irvine
Chair of the Participant Panel
Generating valuable evidence
The NHS blood spot screen (the heel prick test) is used to detect ten rare but serious health conditions in newborn babies. The Generation Study is not intended to replace this important testing which is recommended for all babies.
The Generation Study will generate valuable evidence on whether and how whole genome sequencing should be offered to every baby as part of screening for rare genetic conditions at birth alongside the existing blood spot screen.
The study is for research and includes a specific consent process for parents explaining what to expect and the risks associated with the study. There is a small chance of incorrect or uncertain results. This is the case with any screening programme and because we are still learning about how genetic changes cause disease or ill health. Recognising that receiving a result from the study can be a worrying time for families, Genomics England has worked with the NHS and patient organisations to put supports in place – such as genetic counselling and support groups.
Parents who join the study also agree to their baby’s data being stored in the National Genomic Research Library – a secure national database managed by Genomics England. This data is de-identified and can be accessed by approved researchers from approved institutions, to help improve how we diagnose and treat rare conditions in future. This links to another key aim of the study: supporting broader healthcare research to improve testing and discover more treatments.
Additionally, the study is consulting a range of groups including families, participants and the wider public on exploring the possible risks and benefits of storing a person’s genome and using it throughout their life to help predict, diagnose and treat future illnesses. For example, if a child who has had their genome sequenced falls sick when they are older, there may be an opportunity to use their stored genetic information to help diagnose and treat them.