First newborn babies tested for over 200 genetic conditions as world-leading study begins in NHS hospitals

Hundreds of babies have begun to be tested for over 200 rare genetic conditions as part of a world-leading study in NHS hospitals that aims to screen up to 100,000 newborns in England.
The Generation Study, led by Genomics England in partnership with NHS England, will see newborn babies offered whole genome sequencing using blood samples which are usually taken from their umbilical cord shortly after birth.
The study will identify conditions such as Metachromatic leukodystrophy (MLD) in babies sooner and could enable hundreds to benefit from earlier diagnosis and treatment that could help slow the progression of rare conditions and even extend their lives. It aims to investigate the feasibility and acceptability of using whole genome sequencing to screen newborns for rare conditions where early treatment is available.
Following consultation, the study is only analysing the genomes for the 200 plus selected conditions that can be treated in the NHS in early childhood. It has been developed following extensive consultation with the public, parents and families affected by rare conditions as well as healthcare professionals, policy makers and scientists. This engagement will continue over the course of the study.
Currently, over 1,000 participants have consented to join the study.
Taking part in the study
Expectant parents at participating hospitals will be informed about the study during pregnancy, and if interested a research midwife will have a detailed conversation with them to decide if they want to take part.
Shortly after birth, an NHS doctor, nurse or midwife will confirm with parents that they are still happy for their baby to be tested and a blood sample will be taken and sent to a laboratory for whole genome sequencing.
Results are then reviewed by NHS genomic scientists, with the aim of sharing with parents within 28 days if a condition is suspected or within a few months if no conditions are suspected.
If a newborn baby is identified as having a treatable childhood condition through the genome sequencing, families and carers will be provided with further NHS testing to confirm a diagnosis, and ongoing support and treatment from the NHS.
Study’s launch ‘a pivotal moment’
The Generation Study will also support broader healthcare research to improve testing and discover more treatments. Additionally, it will consult a range of groups including families, participants and the wider public on exploring the possible risks and benefits of storing an individual’s genome over their lifetime and using it to help predict, diagnose and treat future illnesses. For example, if a child who has had their genome sequenced falls sick when they are older, there may be an opportunity to use their stored genetic information to help diagnose and treat them.
“The launch of the Generation Study is a pivotal moment as we look to develop evidence on whether genomic newborn screening should be offered to all children – to do more for the thousands of children born every year in the UK with a treatable genetic condition.
“Children with these conditions often go years without receiving a diagnosis. Cutting this time would mean earlier access to what can be life-changing treatment. The Generation Study also shows the impact of our partnership with the NHS – meaning that the UK is uniquely placed to test, and – where proven – roll out genomic innovations to improve health and help us move healthcare increasingly to preventing illness.”
Dr Rich Scott
Chief Executive Officer at Genomics England
“Diagnosing rare conditions in newborn babies at the earliest opportunity through genomic testing could be truly life-changing for families – it has the potential to give thousands of children the chance to access the right treatment at the right time, giving them the best possible start to life, and for families to better plan for their care.
“The NHS is a world leader in genomics, and this study demonstrates the benefit of our partnership with Genomics England – allowing us to deploy cutting-edge technology to improve patients’ lives. If we can diagnose and treat children for rare genetic conditions years earlier, we have the power to help stop debilitating conditions in their tracks and enable more children to grow up, start school and live independently – this will be transformational for patients and for the future of medicine.”
Amanda Pritchard
NHS Chief Executive
"As a representative of the Genomics England participant panel and someone deeply impacted by rare disease, I believe the Generation Study offers incredible hope. By enabling early diagnosis and treatment for these conditions, we have the potential to transform the lives of countless children and their families. My greatest hope is that this study paves the way for a future where every child, regardless of their genetic makeup, has the opportunity to thrive. This study is a testament to the power of collaboration, innovation, and a commitment to putting patients at the heart of research."
Adam Clatworthy
Vice Chair for Rare Diseases, Genomics England Participant Panel
“To fix our broken NHS, we need to ensure the future of healthcare is more predictive, more preventative and more personalised. This kind of advance in genomics will help us achieve just that – ensuring families across the country have access to the right support and treatment for their loved ones.
“Too many parents are waiting too long for crucial answers on diagnosis, and I am determined that we use innovation to turn that around.”
Wes Streeting
Health and Social Care Secretary
The NHS blood spot screening (the heel prick test) is used to detect nine rare but serious health conditions in newborn babies – the Generation Study is not intended to replace routine screening, and it is important that whatever decision parents make about participation in the Generation Study, their baby still has the blood spot test.
Birth parents who agree to their baby taking part in the Generation Study will have their baby’s data stored in the National Genomic Research Library (NGRL). De-identified genomic and health data in the NGRL can be accessed by approved researchers via a secure research environment.
Earlier access to treatment
One of the first couples to join the Generation Study were Ferne Corrigan and Mark McClean, whose son Caelan has had a sample collected after being born. Ferne and Mark enrolled after a routine scan at St Michael’s Hospital, part of the University Hospitals Bristol and Weston NHS Foundation Trust.
Ferne said: “Both my husband and I felt that contributing to the research was important. Once we realised that our baby’s genome could be used to help others, we put our names down and very much wanted to be a part of that. We also factored in that the study was so non-invasive and that there wouldn’t be much for me to do personally, while still potentially making a difference to people’s lives in the future.”
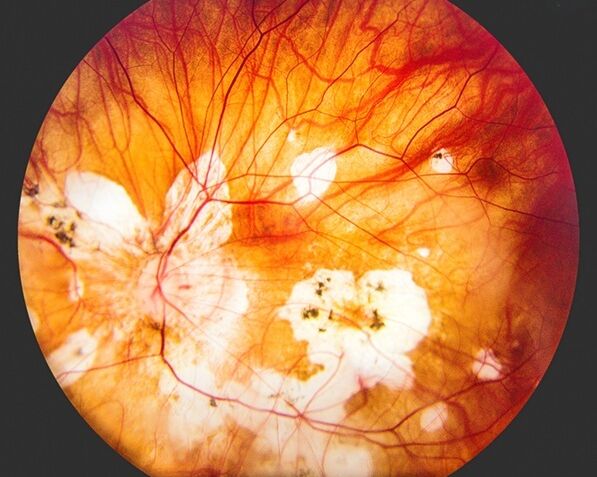
Lucy White’s 9-year-old son Joshua Curtis has Early Juvenile Metachromatic leukodystrophy (MLD), one of the conditions being tested for in the study, she said: “When Josh was born, we had concerns about his mobility, his hand-eye coordination and difficulties he had with swallowing. It took us two years, after many tests and hospital appointments, to get a diagnosis because his condition was so rare. With earlier diagnosis, Josh could have benefitted from transformational gene therapy on the NHS, which would have been life-changing.
“Sadly, it was too late for Josh to receive treatment as his symptoms had progressed too far and he has lost all of the abilities he once had. As a family, the diagnosis of MLD has had a massive impact. I hope that this study will help other families and children access the treatment they need sooner.”